Unlocking Vision: Understanding Everything About Diabetic Macular Edema
Last updated on : 21 Mar, 2025
Read time : 10 min
What is DME?
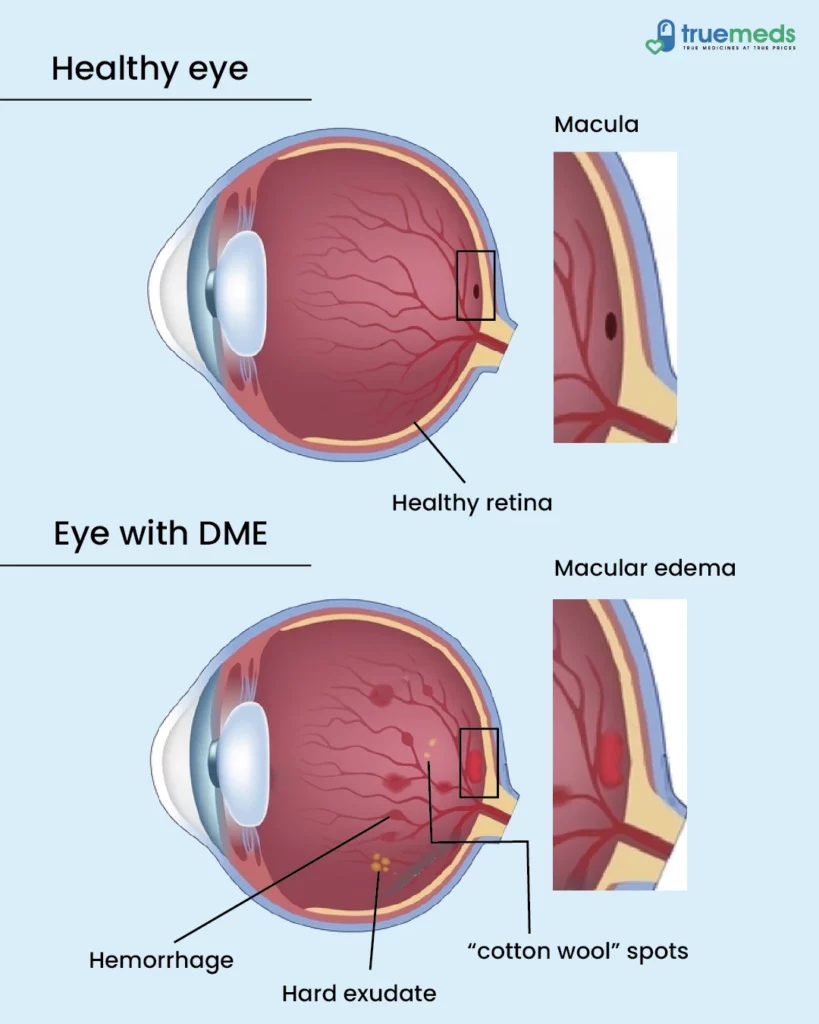
DME stands for Diabetic Macular Edema, a medical condition affecting the eye in individuals with diabetes. DME is a common medical abbreviation for Diabetic Macular Edema.
DME primarily affects the eye, specifically the macula, leading to vision problems and visual disturbances. It happens when fluid accumulates in the central part of the retina (eye), causing blurry vision. Treatment options are available to manage this condition and maintain vision.
Symptoms of Diabetic Macular Edema
Common symptoms of diabetic macular edema include:
- Blurred vision: A typical symptom of diabetic macular edema is blurry vision, which can affect the ability to see fine details.
- Distorted vision: Straight lines may appear wavy or bent, making reading or recognising objects difficult.
- Colour changes: Colors may appear faded or washed out.
- Dark spots: Dark spots or empty spaces may appear in the central vision, obstructing clear sight.
Learn more: Ways to Improve your Eyesight
Causes of Diabetic Macular edema
Various causes of diabetic macular edema include:
- High blood sugar levels: When diabetes is not managed correctly, it can damage the blood vessels in the retina. This damage can cause fluid to leak into the macula.
- Prolonged diabetes duration: Individuals with long-standing diabetes are likely to develop diabetic macular edema.
- Poor diabetes management: Inadequate blood sugar levels, blood pressure, and cholesterol control can increase the likelihood of macular edema in diabetics.
Types of Diabetic Macular Edema
Most typical types of DME include
Early diabetic macular edema
It is the initial stage of diabetic macular edema, where mild swelling and fluid buildup occur in the macula (a small, specialised area near the retina’s central region, the light-sensitive tissue in the eye). It may not cause noticeable vision problems initially, but early detection and management are essential to prevent progression.
Simple diabetic macular Edema
The macula has moderate swelling in this type, leading to blurred or distorted vision. It may affect both eyes and can worsen over time if left untreated. Regular monitoring and proper management of diabetes are crucial for controlling this type.
Cystoid diabetic macular edema
Cystoid diabetic macular edema is characterised by the formation of fluid-filled cysts in the macula, causing significant vision loss. It can result in distorted or blurry central vision. Fast diagnosis and treatment are essential to prevent further damage and preserve vision.
The Risk Factors for Diabetic Macular Edema
- Poor blood sugar management: Inadequate control of blood sugar levels increases the risk of developing DME.
- High cholesterol: Elevated cholesterol levels can contribute to the development of DME in individuals with diabetes.
- High blood pressure: Unchecked high blood pressure is a risk factor for DME.
- Kidney disease (nephropathy): Individuals with kidney disease associated with diabetes have a heightened risk of developing DME.
Learn more: How to Improve your Kidney Health
Diagnosing Diabetic Macular edema
At Home
It is impossible to diagnose DME at home. If you are experiencing signs or are at risk, seeing an eye specialist for a proper diagnosis is essential.
Learn more: Home remedies for Eye Infection
Eye Exams
Eye exams are essential for diagnosing DME. An eye specialist will examine your eyes using various tests and tools to determine if you have DME and assess the severity.
Tests for DME
Tests used to diagnose DME may include optical coherence tomography (OCT), which creates detailed retina images, and fluorescein angiography, which involves injecting a dye into your arm to highlight blood vessels in the eye and detect abnormalities. These tests help the eye specialist make an accurate diagnosis and determine the appropriate treatment.
How to Prevent DME
Strategies for the prevention of the DME includes
- Discuss treatment options with your doctor: It’s always possible to start treatment for DME. Acting quickly can prevent long-term eye damage.
- Schedule annual eye checkups: Regular doctor visits can help detect changes in your vision and ensure timely intervention.
- Act on vision changes promptly: If you notice any changes, contact your eye care doctor immediately for evaluation and guidance.
- Manage blood sugar levels: Work closely with your doctor to effectively control your blood sugar levels, which can help prevent complications.
Learn more: Eye Care Tips
Diabetic macular edema treatments
Various treatments that help manage DME include
1) Laser photocoagulation
This treatment uses a laser to seal leaking blood vessels in the retina, reducing swelling and preventing further vision loss. It is commonly used for focal macular edema.
2) Corticosteroids
Corticosteroids can be injected into the eye to decrease inflammation and reduce macular edema. They help to control the swelling and improve vision, but their effects may be temporary.
3) Anti-VEGF therapy
Injections of anti-VEGF drugs block the growth of abnormal blood vessels and reduce fluid leakage in the macula. This treatment has shown promising results in improving vision and preventing further damage in patients with diabetic macular edema.
4) mTOR inhibitors
mTOR inhibitors are a class of medications that can treat diabetic macular edema by inhibiting specific cell signalling pathways involved in abnormal blood vessel growth and inflammation in the retina. They have shown potential in reducing macular edema and improving visual acuity.
5) Protein kinase C
Inhibition of protein kinase C, an enzyme involved in various cellular processes, has been investigated as a potential treatment for diabetic macular edema. Targeting this enzyme is hoped to reduce inflammation and prevent blood vessel leakage in the retina.
6) Ras/Raf/Mek/Erk
This signalling pathway plays a role in the development of diabetic macular edema. Inhibitors targeting specific components of this pathway are being studied as potential treatments to suppress abnormal blood vessel growth and decrease retinal inflammation.
7) ICAM-1
ICAM-1 is a cell adhesion molecule involved in the inflammatory process. Targeting ICAM-1 may help reduce the adhesion of inflammatory cells in the retina and alleviate macular edema.
8) MMPs
Matrix metalloproteinases (MMPs) are enzymes that contribute to the breakdown of the matrix in the retina. Inhibiting MMPs may help reduce the breakdown of the blood-retinal barrier and prevent fluid accumulation in the macula.
9) Nicotinic acetylcholine receptor
Activation of nicotinic acetylcholine receptors has shown potential in reducing inflammation and preventing blood vessel leakage in diabetic macular edema. Modulating these receptors may help in improving macular edema and preserving vision.
10) Receptor for Advanced Glycation End-Products
Inhibition of the receptor for advanced glycation end-products (RAGE) has been studied as a potential therapeutic target for diabetic macular edema. By blocking RAGE, it is hypothesised to reduce inflammation and vascular leakage in the retina.
11) Renin-angiotensin system
Medications that target the renin-angiotensin system, such as angiotensin-converting enzyme (ACE) inhibitors and angiotensin receptor blockers (ARBs), are commonly used to manage conditions like high blood pressure. It can also affect diabetic macular edema by reducing inflammation and improving blood flow in the retina.
12) Combined Therapies
Different treatments may sometimes be used to manage diabetic macular edema. This approach may involve a combination of laser photocoagulation, anti-VEGF therapy, corticosteroids, or other targeted therapies to achieve better outcomes in reducing macular edema and improving vision.
Conclusion
Diabetic macular edema (DME) can be managed with various treatments. It is possible to maintain or even regain vision. Detecting DME early can help prevent vision loss. Regular visits to your eye care doctor are crucial for eye health and overall well-being.
You can download our user-friendly Truemeds app for easy access to medicine at low rates. Submit your prescription to our platform to receive branded and generic medications. Enjoy savings on purchases and the added convenience of free home delivery on relevant orders across India*.
Frequently asked questions
While natural remedies cannot cure diabetic macular edema (DME), maintaining reasonable blood sugar control through a healthy diet, regular exercise, and medication adherence can help manage the condition.
Vision restoration in diabetic macular edema depends on the severity and timely treatment. Early detection and appropriate interventions, such as anti-VEGF injections or laser therapy, can sometimes improve vision.
The first line of management for diabetic macular edema often involves anti-VEGF injections, which help reduce swelling and improve vision. Other treatments like laser photocoagulation or corticosteroid injections may also be considered based on individual needs.
Certain medications used to manage systemic conditions like hypertension or diabetes can potentially contribute to diabetic macular edema. However, the condition is primarily associated with underlying diabetes itself.
Diabetic macular edema can be a chronic condition, but it is possible to control and minimise its impact on vision with appropriate treatment and management. Regular follow-up with healthcare professionals is essential to monitor and manage the condition effectively.
While Ayurveda offers alternative approaches to managing various health conditions, consulting with a qualified Ayurvedic practitioner or healthcare provider is essential to discuss potential treatments and their efficacy for diabetic macular edema.
Laser therapy, specifically laser photocoagulation, is a standard treatment for diabetic macular edema. The laser is used to close leaking blood vessels and reduce swelling in the macula, which can help improve vision and slow down the condition’s progression.
A balanced and healthy diet is necessary for managing diabetic macular edema. It typically includes foods rich in antioxidants, such as fruits, vegetables, grains, proteins, and healthy fats. Consulting a registered dietitian or nutritionist can provide personalised dietary recommendations.
While specific vitamins are not proven to cure diabetic macular edema, specific vitamins and minerals, such as vitamin C, E, zinc, and omega-3 fatty acids, may benefit eye health. It is vital to discuss any supplements with a healthcare professional.
Turmeric, known for its anti-inflammatory properties, may have potential health benefits. While research on its direct effect on diabetic macular edema is limited, incorporating turmeric into a balanced diet may contribute to overall well-being. Consult with a healthcare professional before using turmeric or any supplements.
Disclaimer
The content provided within this article has been thoroughly verified for accuracy. However, we advise consulting a healthcare professional before utilising any medication or dietary supplements mentioned herein.
References
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3277023/
- https://www.hindawi.com/journals/jdr/2015/794036/
- https://eyewiki.aao.org/Diabetic_Macular_Edema
- https://www.sciencedirect.com/science/article/pii/S0039625708001811
- https://cellandbioscience.biomedcentral.com/articles/10.1186/2045-3701-4-27#Sec24
Disclaimer
Our healthcare experts have carefully reviewed and compiled the information presented here to ensure accuracy and trustworthiness. It is important to note that this information serves as a general overview of the topic and is for informational purposes only. It is not intended to diagnose, prevent, or cure any health problem. This page does not establish a doctor-patient relationship, nor does it replace the advice or consultation of a registered medical practitioner. We recommend seeking guidance from your registered medical practitioner for any questions or concerns regarding your medical condition.
Popular Articles
Recommended Articles
Recent Articles
Top-Selling Medicines:
...View more
Top-Selling OTC:
...View more
Company
About UsHealth ArticleHealth StoriesDiseases & Health ConditionsAll MedicinesAll BrandsNeed HelpFAQSubscribe
Registered Office Address
Grievance Officer
Download Truemeds

Contact Us
Our customer representative team is available 7 days a week from 9 am - 9 pm.
v3.7.11
Our Payment Partners



























































